20 Rare Mental Disorders

Delve into the captivating realm of rare mental disorders, where the boundaries of human psychology are tested and redefined. Explore 20 of these enigmatic conditions, each characterized by unique symptoms, causes, and challenges. From the distorted perceptions of Alice in Wonderland Syndrome to the uncontrollable hair-pulling of Trichotillomania, each disorder unveils a fascinating facet of the human mind. Embark on a journey of understanding, shedding light on these often misunderstood conditions and the individuals who courageously navigate their complexities.
Alice in Wonderland Syndrome
Alice in Wonderland Syndrome is a rare mental disorder that affects the brain’s ability to process sensory information, leading to perceptual distortions. AIWS can cause a person to perceive their own body or objects around them as smaller or larger than they actually are. The exact cause of AIWS is unknown, but it is often associated with migraines, infections, and other neurological conditions. However, the good news is that AIWS is usually a temporary condition, and treatment primarily involves addressing the underlying cause. People with AIWS can lead normal, healthy lives with proper diagnosis and treatment.
Cotard’s Delusion Disorder
Delusion include intense delusions of negation, chronic psychiatric depression, and self-loathing. While the exact cause of Cotard’s Delusion is not clear, it is often associated with conditions such as dementia, encephalopathy, multiple sclerosis, Parkinson’s disease, stroke, subdural bleeding, epilepsy, and migraine. The treatment for Cotard’s Delusion typically involves addressing the underlying cause, with most individuals responding well to a combination of medication and cognitive behavioral therapy (CBT) or psychotherapy.
Erotomania Mental Disorder
Erotomania, which is also known as De Clérambault’s Syndrome, is a rare psychiatric disorder that affects an individual’s perception of reality. Holding a delusional belief that someone of higher social status is deeply in love with them is a symptom of this disorder. Common symptoms of Erotomania include obsessive behaviors and elaborate fantasies directed towards the object of their affection.
The exact cause of this disorder is still not clear, but it is often related to other psychiatric diseases such as schizophrenia, bipolar disorder, and major depressive disorder. Fortunately, treatment is possible for those who suffer from Erotomania. A combination of therapy and medication, particularly cognitive-behavioral therapy (CBT) and antipsychotic medications, are the most common forms of treatment.
Geschwind Syndrome
Geschwind Syndrome is a behavioral condition that is observed in some people who have temporal lobe epilepsy. It is also known as Gastaut-Geschwind syndrome. The disease is characterized by several symptoms, such as hypergraphia (a tendency to write excessively), hyperreligiosity (intense religious feelings), atypical sexuality (usually reduced), circumstantial, and intensified mental life.
Although the exact cause of the condition is unknown, it is often associated with temporal lobe epilepsy. Treatment for Geschwind Syndrome primarily involves addressing the underlying cause. In some cases, temporal lobe resection, a surgery that eliminates the seizure focus, may be used. Symptomatic and supportive treatments, such as occupational and speech therapies, may also help manage the symptoms.
Kleptomania
Kleptomania is a mental disorder characterized by an irresistible urge to steal items, often of little or no value. Before theft, individuals with kleptomania may experience feelings of tension, followed by pleasure or relief afterward. The exact cause of Kleptomania is not known, but it may be linked to imbalances in brain neurotransmitters, genetics, and the presence of other psychiatric conditions.
Treatment options for kleptomania typically include a combination of psychotherapy and medication, such as cognitive-behavioral therapy (CBT) and selective serotonin reuptake inhibitors. If you or someone you know is struggling with kleptomania, it is important to seek professional help from a mental health provider.
Morgellons Disease:
Morgellon disease is a rare and mysterious medical condition often controversial and poorly understood. One of the most common symptoms of this condition is the development of skin lesions and the appearance of fibers under or protruding from the skin. Individuals with Morgellons disease also report crawling or stinging sensations under the skin. While the exact cause of this condition is unclear, it may be associated with Lyme disease or considered a form of psychosis.
Treatment for Morgellons Disease varies depending on the perceived underlying cause and may include antibiotics, antipsychotics, or cognitive behavioral therapy. It is important to note that a strong patient-doctor relationship is crucial for effectively managing this condition.
Munchausen Syndrome
Munchausen Syndrome is a rare mental health condition that affects individuals who falsify, exaggerate, or induce physical, emotional, or cognitive disorders. People with this disorder may lie about their symptoms, tamper with medical tests, or self-harm to produce symptoms. The actual cause of this disorder is not clear. However, researchers believe it is related to past traumatic experiences, such as abuse or neglect. Treatment for this disorder primarily involves psychotherapy, particularly cognitive-behavioral therapy (CBT), which focuses on changing the individual’s thoughts and behavior.

Obsessive-Compulsive Personality Disorder
Ever come across the term Obsessive-Compulsive Personality Disorder (OCPD)? If your answer is no, you’re not alone. Despite being a common condition, OCPD remains a mystery to many. This write-up seeks to demystify OCPD, shedding light on its symptoms, likely causes, diagnosis process, and possible treatment avenues.
Obsessive-Compulsive Personality Disorder is a personality disorder that’s marked by an overarching preoccupation with orderliness, perfection, and control. This often comes at the expense of flexibility, openness, and efficiency. Mind you, OCPD shouldn’t be confused with Obsessive-Compulsive Disorder (OCD), even though their names might suggest a connection.
People grappling with OCPD are usually high achievers who take their responsibilities seriously. But, their excessive focus on minutiae, rules, and schedules can lead to inefficiency and stress. Their staunch adherence to routines and their perfectionist tendencies can strain relationships and impede their ability to adapt to change.
What triggers OCPD remains a mystery. It’s widely believed, though, that it stems from genetic, environmental, and psychological elements. Some studies hint that having parents with rigid personality styles or growing up in a home where high standards and rules were excessively emphasized could lead to the onset of OCPD.
Diagnosing OCPD calls for a comprehensive evaluation by a mental health professional. This evaluation usually includes an exhaustive interview and an analysis of the individual’s history. The diagnosis hinges on the individual’s recounted experiences, as well as observations and assessments made by the professional.
While there’s no known cure for OCPD, there are many treatment options that can help control the symptoms and improve the quality of life. Cognitive-behavioral therapy (CBT) is seen as the most effective form of treatment. It allows individuals with OCPD to challenge their perfectionistic and inflexible beliefs, learn to ease their standards and become more receptive to change.
Medication is generally not the first choice of treatment for OCPD. However, in certain cases, antidepressants or other psychiatric medications might be recommended, particularly if the individual is also battling another mental health disorder like anxiety or depression.
Support from family, social circle, and mental health professionals can be a lifeline for individuals navigating the choppy waters of life with OCPD. Joining a support group can also foster a sense of community and understanding, ensuring individuals don’t feel alone in their experiences.
In summary, Obsessive-Compulsive Personality Disorder is a complex condition that can significantly shape an individual’s life. However, with understanding, treatment, and support, individuals with OCPD can learn to manage their symptoms and lead fulfilling lives. If you or someone you know is wrestling with symptoms of OCPD, don’t hesitate to seek professional help. Remember, reaching out for help is the first step on the road to recovery.
Pica
Do you ever feel like munching on something that’s not food? You may have caught yourself chewing on ice, paper, or even clay. If so, you might be experiencing a condition known as pica.
Pica is not a fancy name for a type of food; it’s an eating disorder characterized by the persistent consumption of non-nutritive substances. People with pica crave items without nutritional value, such as dirt, chalk, hair, soap, or metal objects. These cravings can be intense and challenging, leading to potentially harmful consequences.
Pica’s presence can be traced back thousands of years across various cultures and civilizations. Ancient Greek and Roman texts mention individuals consuming unusual substances such as dirt or clay. In some cultures, ingesting specific non-food items was believed to possess medicinal or spiritual benefits.
During the Middle Ages, pica was often associated with superstition and considered a sign of demonic possession or moral weakness. People believed that those who indulged in such cravings were under the influence of evil spirits or cursed by divine punishment.
As scientific understanding developed, pica was recognized as a medical condition rather than a supernatural occurrence. However, misconceptions and stigma surrounding the disorder persisted well into modern times.
While precise data on the prevalence of pica is limited, studies suggest that it remains a relatively rare condition in the general population. However, specific demographics, such as children, pregnant women, and individuals with developmental disabilities, are more likely to experience pica.
Among pregnant women, pica cravings are particularly common, with estimates suggesting that up to 25% may engage in the consumption of non-food items such as ice, clay, or laundry starch. During pregnancy, hormonal changes and nutritional deficiencies can cause cravings for non-food items, a condition known as gestational pica.
In children, pica may occur as a developmental phase, typically between 1 and 6, when exploration and oral fixation are expected behaviors. Most children outgrow these behaviors without intervention, but permanent or severe cases may require medical attention.
Among individuals with developmental disabilities or psychiatric disorders, the prevalence of pica is higher compared to the general population. In these cases, pica may be associated with sensory issues, cognitive impairments, or compulsive behaviors.
Our understanding of pica has come a long way since ancient times, thanks to medical science and research advances. Today, pica is recognized as a complex disorder with multifaceted causes and potential consequences for physical and mental health.
Treatment approaches for pica have also evolved, moving from traditional beliefs and superstitions to evidence-based interventions. Behavioral therapies help individuals with pica learn alternative behaviors and coping strategies.
Nutritional counseling and supplementation are crucial in addressing underlying deficiencies contributing to pica cravings. By ensuring adequate intake of essential nutrients, healthcare providers can help reduce the likelihood of cravings for non-food items.
In cases where pica is associated with underlying mental disorders, the medicine may be prescribed to manage symptoms and improve overall well-being.
Pica may have ancient origins, but our understanding of this condition has evolved significantly. Providing appropriate treatment and support for pica as a medical disorder can help individuals overcome cravings for non-food items and improve their quality of life. Through continued research and education, we can strive to destigmatize pica and ensure those affected receive the care and understanding they deserve.
Prader-Willi Syndrome
Did you know that Prader-Willi Syndrome (PWS) is a genetic disorder that affects different parts of the body? It’s a complex condition that can cause various symptoms, and there’s still much to learn about it. It is a rare disorder caused by the absence of active genetic material in a specific region of chromosome 15. PWS can cause several symptoms, including poor muscle tone, distinct facial features, poor sucking reflex, lethargy, and underdeveloped genitals in infants.
As the child grows, symptoms such as excessive hunger, obesity, underdeveloped sex organs, poor growth, intellectual disability, speech problems, behavioral issues, sleep disorders, and physical deformities may occur. However, the good news is that several therapies, such as growth hormone therapy, hormone therapy, sleep disturbance therapy, behavioral therapy, physiotherapy, speech therapy, and developmental therapy, can help manage the symptoms of PWS.
Prosopagnosia
Prosopagnosia, often referred to as face blindness, is a rare neurological condition that affects a person’s ability to recognize faces. While it might seem like a niche topic, the impact of prosopagnosia extends far beyond mere facial recognition. In this article, we delve into the intricacies of prosopagnosia, exploring its causes, symptoms, and the challenges individuals face. Additionally, we’ll highlight some coping mechanisms and recent research advancements in the field.
Imagine a world where every face looks unfamiliar, and distinguishing between your closest friends and strangers becomes arduous. This is the reality for individuals with prosopagnosia. Stemming from various factors such as brain injury, genetics, or developmental abnormalities, prosopagnosia disrupts the brain’s ability to process and recognize faces.
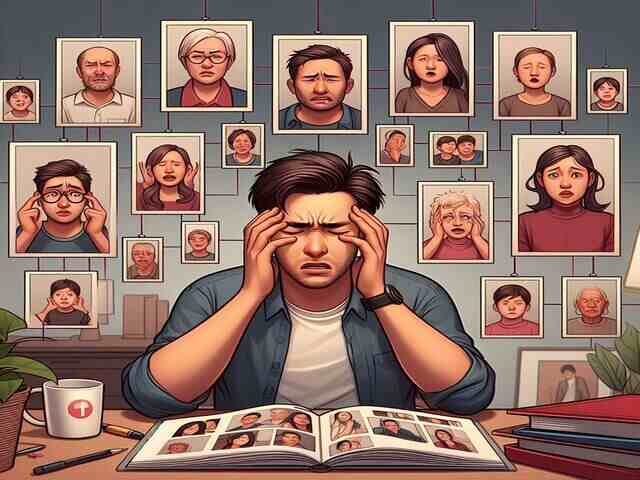
Living with prosopagnosia presents a myriad of challenges in both personal and professional spheres. Superficial social interactions can become daunting tasks, leading to feelings of isolation and anxiety. Recognizing family members, navigating crowded places, or watching movies can evoke frustration and inadequacy.
Despite the challenges posed by prosopagnosia, individuals often develop coping mechanisms to navigate the world around them. They compensate for their inability to rely on facial recognition by utilizing alternative cues such as voice, gait, or contextual clues. Additionally, technology has played a pivotal role in assisting individuals with prosopagnosia, with facial recognition apps and specialized training programs offering support and assistance.
One of the most significant hurdles faced by individuals with prosopagnosia is the lack of awareness and understanding from society. Misconceptions and stigma surrounding the condition can lead to feelings of alienation and misunderstanding. By fostering awareness and education, we can create a more inclusive environment where individuals with prosopagnosia feel supported and understood.
While there is currently no cure for prosopagnosia, ongoing research holds promise for improved diagnosis and treatment options. Advances in neuroimaging techniques and cognitive therapies offer hope for individuals seeking to manage their condition more effectively. By unraveling the complexities of prosopagnosia, researchers aim to provide targeted interventions and support for those affected by this condition.
Prosopagnosia is more than an inability to recognize faces—it’s a complex neurological condition that impacts every aspect of a person’s life. Increasing awareness, fostering understanding, and supporting ongoing research can empower individuals with prosopagnosia to navigate the world with confidence and resilience. Let us strive to create a society where differences are celebrated and everyone feels seen and valued, regardless of their ability to recognize faces.
Restless Legs Syndrome
Have you ever tried to fall asleep only to be kept awake by a peculiar feeling in your legs, urging them to move? It’s as if they’ve decided to dance when you yearn for stillness. You could be one of the many worldwide grappling with Restless Legs Syndrome (RLS).
Restless Legs Syndrome, also known as Willis-Ekbom disease, is a condition where individuals feel an irresistible need to move their legs. Imagine a swarm of ants marching relentlessly under your skin or the sensation of bubbly soda pop coursing through your veins. This is how some describe their experience.
The cause of Restless Legs Syndrome continues to puzzle us. However, it seems to have links to imbalances in dopamine, a substance that helps us move smoothly. Other factors might include inherited traits, pregnancy, and certain medicines.
The cover of darkness often brings a rise in Restless Legs Syndrome symptoms, which can disrupt sleep and affect overall health and everyday activities. If your sleep is being stolen by a constant need to move your legs, it’s time to seek medical advice.
Diagnosing Restless Legs Syndrome often depends on the individual’s specific symptoms. Doctors look for key signs, like an uncomfortable feeling accompanied by a need to move the legs, symptoms that worsen with inactivity and get better with movement, and a spike in symptoms in the evening or night.
While Restless Legs Syndrome may not have a known cure, there are ways to manage the symptoms. This includes changes in lifestyle, physical therapy, and doctor-recommended medicines. Regular exercise, eating well, and avoiding things like caffeine and alcohol can significantly ease RLS symptoms.
Doctor-recommended medicines for Restless Legs Syndrome usually aim to restore dopamine balance or influence calcium channels to lessen muscle spasms. These medicines should be used with caution due to potential side effects.
Other soothing treatments such as leg massages, warm baths, and using heat and cold packs can also provide relief. Proper sleep habits are another important part of managing RLS. Following a regular sleep schedule and creating a quiet, comfortable sleep environment can make a world of difference.
Living with Restless Legs Syndrome is undeniably tough, but remember, you’re not alone. Many are on the same sleepless journey, seeking answers. Joining support groups, sharing experiences, and learning from others who understand your struggle can be hugely helpful.
In essence, Restless Legs Syndrome may be a silent discomfort, but it doesn’t have to rule your life. With the right information, support, and treatment plan, you can manage your symptoms and take back control of your nights. Don’t let Restless Legs Syndrome steal another night’s rest. After all, rest should be peaceful, not restless.
Rett Syndrome
Rett Syndrome is a neurological disorder that mainly affects females. The disease is caused by a mutation of the MECP2 gene on the X chromosome. The symptoms of Rett Syndrome include slowed growth, repetitive jerky movement of limbs, delayed speech, loss of communication skills, seizures, irregular heartbeat and breathing, scoliosis, abnormal muscle stiffness, sleep disorders, and gastrointestinal problems.
There are different treatment options available for managing the symptoms of Rett Syndrome. Medications like Propranolol, Sodium valproate, and Olanzapine are used to manage the symptoms. If you or a loved one is dealing with a disorder, several therapies can help in the recovery process.
Physical, occupational, and speech and language therapy can greatly improve one’s overall well-being and quality of life. These therapies help individuals regain strength, mobility, and communication skills. They can be changed to meet each person’s unique needs and goals, making them an effective way to address specific health challenges. With the right therapy and support, it is possible to overcome the difficulties of a disorder and live a fulfilling life. If you know anyone with Rett Syndrome, it is important to understand the condition and help them manage their symptoms.
Schilder’s Disease
Have you ever heard of Schilder’s Disease? Don’t feel alone if you haven’t. This rare neurological disorder is as elusive as it is severe, often leaving the medical community perplexed and families affected by it grappling for answers. This article aims to shed light on Schilder’s Disease, demystifying its symptoms, causes, diagnosis, and treatment options.
Schilder’s Disease, also known as myelinoclastic diffuse sclerosis, is a rare progressive demyelinating disorder. In simpler terms, it’s a condition where the protective covering of nerve cells in the brain, called myelin, is damaged. This damage slows down the transmission of messages between the brain and the body, leading to neurological symptoms.
Symptoms of Schilder’s Disease can vary widely from person to person, but they often resemble those seen in multiple sclerosis. They may include headaches, nausea, difficulty with balance and coordination, hearing loss, and behavioral changes. These symptoms can be sudden and may progress rapidly, making early diagnosis critical.
So, what causes Schilder’s Disease? The truth is, we don’t know for sure. Some studies suggest it may be an autoimmune disorder in which the body kills its cells. Others believe it could be linked to viral infections. However, more research is needed to clarify these theories.
Diagnosing Schilder’s Disease is a challenge due to its rarity and similarity to other conditions. It often involves a process of elimination, ruling out other diseases through various tests, including magnetic resonance imaging (MRI). An MRI can help identify the characteristic large, symmetrical lesions in the brain associated with Schilder’s Disease.
There’s no specific cure for Schilder’s Disease, but there are techniques to control and slow disease progression. These can include medications to reduce inflammation and improve the immune response, physiotherapy to help with movement problems, and counselling to manage mental health issues that may arise.
While navigating life with Schilder’s Disease can be daunting, it’s important to remember that you are not alone. Support from family, friends, and healthcare professionals can be crucial. Consider joining a support group to connect with others facing similar challenges and share experiences.
In conclusion, while Schilder’s Disease may be a rare and complex condition, knowledge about it is power. Understanding the Disease, its symptoms, and the available treatments is the first step towards managing it effectively. If you or a loved one are experiencing symptoms, don’t hesitate to seek medical advice. “Early diagnosis and intervention can play a crucial role in managing Schilder’s Disease. It’s important to catch and address the Disease early.”
Despite the challenges, many people with Schilder’s Disease lead fulfilling lives, proving that the Disease may change the course of life, but it doesn’t define it. With the right care, support, and treatment, you can navigate the journey of living with Schilder’s Disease.

Stendhal Syndrome
Ever stood in front of a captivating piece of art and felt your heart flutter, knees buckle, or even a sense of faintness? If so, you might have had a brush with Stendhal Syndrome, a curious phenomenon where art induces profound emotional responses. This article seeks to navigate the intriguing waters of Stendhal Syndrome, discussing its symptoms, potential origins, the science behind it, and its position in our modern world.
Stendhal Syndrome, named after the French author who first chronicled it in the 19th century, is a unique reaction to witnessing art. People experiencing it may display a host of symptoms, from rapid heartbeat and dizziness to fainting spells. In acute cases, they may even suffer from hallucinations or bouts of temporary insanity. Although any art can trigger it, it’s most commonly linked with the awe-inspiring beauty of art in Italian cities like Florence.
What actually causes Stendhal Syndrome is still a mystery. Some theories propose it’s a result of an intensely emotional reaction to beauty. In contrast, others suggest it could be due to the overwhelming sensation of being surrounded by an abundance of magnificent art.
Diagnosing Stendhal Syndrome is a challenge, given it doesn’t conform to standard medical classifications. It’s typically identified through the individual’s reported experiences and symptoms following art exposure. Notably, it’s not officially recognized as a disorder by the broader medical community.
Despite its elusive nature, some research has attempted to demystify the science behind Stendhal Syndrome. Studies propose it might be connected to the release of dopamine in the brain which is associated with pleasure and reward when viewing art. This dopamine rush could trigger the intense emotional and physical reactions seen in Stendhal Syndrome.
In today’s world, Stendhal Syndrome is viewed through various lenses. Some see it as an extreme form of artistic appreciation, a testament to the profound emotional impact art can have. Others, however, consider it a fascinating peculiarity, a psychological quirk that blurs the boundaries between art, emotion, and physical health.
Though there’s no specific treatment for Stendhal Syndrome, those who experience it are often advised to limit their art exposure and take breaks during museum visits. In more severe cases, psychological support or counseling may be recommended.
To conclude, Stendhal Syndrome remains a captivating crossroad between art and psychology. It might seem perplexing to some, but it underscores the remarkable power art wields over our emotions, thoughts, and even our physical well-being. If you, or someone you know, experience overwhelming reactions to art, it could be intriguing to delve deeper into the compelling world of Stendhal Syndrome. Remember, art is meant to stir us, to evoke emotions, and in the case of Stendhal Syndrome, it does so with a potency that can leave us breathless.
Tourette Syndrome
Tourette Syndrome is a mental disorder that often grabs headlines for its portrayal in the media, but do we truly understand what it entails? This article aims to provide an insightful and comprehensive overview of Tourette Syndrome, including its symptoms, causes, diagnosis, and available treatments.
Tourette Syndrome is a complex condition characterized by involuntary movements and vocalizations known as tics. These tics can range from mild, such as eye blinking or throat clearing, to more severe, such as repetitive arm jerking or uncontrollable shouting of words or phrases. Remember, all individuals with Tourette Syndrome do not experience the same tics or exhibit them constantly.
The causes of Tourette Syndrome may involve a combination of genetic and environmental factors. Evidence supports the involvement of certain genes that affect the brain’s neurotransmitters, specifically dopamine. However, more research is needed to understand the underlying mechanisms fully.
Diagnosis of Tourette Syndrome can be difficult because there is no specific medical test for it. Doctors rely on observing the presence, frequency, and duration of both motor and vocal tics. It’s also important to rule out other potential causes of the tics, such as medication side effects or other medical conditions.
Living with Tourette Syndrome can be difficult because of the social stigma and misconceptions associated with the condition. It’s crucial to create an inclusive and understanding environment for individuals with Tourette Syndrome, where they feel supported and accepted.
While there is no cure for Tourette Syndrome, different treatment methods can help manage the symptoms and improve quality of life. Behavioral therapy can guide individuals to recognize and control their tics. Medications may also be prescribed to reduce the frequency and severity of tics when needed.
Support from family, friends, and support groups can be immensely valuable for individuals with Tourette Syndrome. Education and awareness about Tourette Syndrome in schools and groups can help reduce fear and improve understanding.
In conclusion, Tourette Syndrome is a complex neurological condition that affects individuals in unique ways. A deeper understanding of the disorder and promoting empathy and acceptance can create a more inclusive society for those living with it. Let’s challenge misconceptions, support research efforts, and provide an environment where individuals with Tourette Syndrome can thrive and be understood.
Remember, the condition itself does not define the journey of living with Tourette Syndrome; it is defined by each individual’s strength, resilience, and unique qualities.
Trichotillomania
Have you ever found yourself absentmindedly playing with your hair, tugging at a strand or two? It’s a common habit for many, but for some, this seemingly harmless act can escalate into a serious condition known as Trichotillomania. .
Trichotillomania, also known as hair-pulling disorder, is a mental health condition where individuals grapple with an uncontrollable urge to pull out their hair. This can be from any part of the body, but it’s usually the scalp, eyebrows, and eyelashes that bear the brunt. The act of pulling, often a response to feelings of anxiety or tension, can lead to noticeable hair loss and significant emotional distress.
People living with Trichotillomania often find themselves on an emotional rollercoaster. The act of pulling provides a temporary respite from anxiety, but it’s usually followed by feelings of guilt and embarrassment, leading many to hide their condition from others.
The exact cause of Trichotillomania is still a subject of ongoing research. Current theories suggest a mix of genetic, environmental, and neurological factors. Some studies indicate differences in the brain circuits that regulate impulse control and habits. However, a definitive cause is yet to be pinpointed.
Diagnosing Trichotillomania can be tricky due to its secretive nature. Many individuals keep their hair-pulling a secret due to fear of judgment.
While there’s no specific cure for Trichotillomania, several treatment options can help manage the symptoms. Cognitive-behavioral therapy (CBT) is often the first step. It allows professionals to understand their triggers and develop healthier coping mechanisms.
Living with Trichotillomania can feel isolating, but it’s crucial to remember that support is within reach. Support groups, whether online or in person, offer a secure environment for sharing experiences, gaining insights from others, and alleviating feelings of isolation.
In conclusion, Trichotillomania is not just a hair-pulling disorder. It’s a complex condition that permeates every aspect of an individual’s life. If you or someone you know is wrestling with Trichotillomania, remember that help is available.
Remember, Trichotillomania doesn’t define you or limit your potential. With the right treatment and support, it’s entirely possible to overcome the urge to pull and regain control of your life. So, let’s continue raising awareness, combating stigma, and supporting those who are silently battling this often unseen struggle.
Visual Snow Syndrome
Visual Snow Syndrome is a rare disorder that causes individuals to see continuous, tiny, moving dots throughout their entire visual field, which can distract and interfere with daily activities. People with this condition may experience visual disturbances such as “snow” or “static” that appear everywhere, whether their eyes are open or closed.
The exact cause of Visual Snow Syndrome is not fully understood, but it may be linked to increased excitability in the occipital lobes of the brain where images are processed. Unfortunately, there is no established cure for this disorder, but medications such as lamotrigine, acetazolamide, or verapamil have been used to manage symptoms. If you or anyone you know is experiencing symptoms of Visual Snow Syndrome, consult a qualified healthcare professional for proper diagnosis and management.
Wernicke-Korsakoff Syndrome
Wernicke-Korsakoff Syndrome (WKS) is a serious neurological disorder caused by a deficiency in thiamine (vitamin B1). It is most commonly associated with chronic alcohol abuse but can also result from malnutrition or other conditions that impede thiamine absorption.
WKS is two separate conditions that often occur together: Wernicke’s encephalopathy and Korsakoff’s psychosis. Wernicke’s encephalopathy is the acute phase, marked by confusion, lack of coordination, and abnormal eye movements. If untreated, it can progress to Korsakoff’s psychosis, a chronic condition characterized by severe memory problems, difficulty forming new memories, and confabulation (fabricating stories to fill memory gaps).
The primary cause of WKS is a severe thiamine deficiency, which is essential for brain function. Chronic alcohol consumption is a leading cause because alcohol interferes with thiamine absorption and storage. Other risk factors include eating disorders, prolonged vomiting, and conditions like AIDS.
Early diagnosis and treatment are crucial for WKS. Immediate administration of thiamine can alleviate symptoms of Wernicke’s encephalopathy and prevent progression to Korsakoff’s psychosis. However, recovery from the chronic stage is often partial, with many patients experiencing lasting cognitive deficits.
Raising awareness about Wernicke-Korsakoff Syndrome is essential for early intervention and prevention. Ensuring adequate thiamine intake, particularly in at-risk populations, can help reduce the incidence of this debilitating disorder. Understanding and supporting those affected by WKS can improve their quality of life and promote better health outcomes.
Wilson’s Disease
Wilson’s Disease causes the accumulation of traces of copper present in crucial organs like the liver and brain. The Disease is caused by a mutation in the ATP7B gene. Symptoms of the Disease include tiredness, loss of appetite, jaundice, fluid buildup in the legs or stomach area, problems with speech, swallowing or physical coordination, depression, mood changes, and personality changes.
Treatment for Wilson’s Disease involves medications like Penicillamine and Trientine, which help the body’s organs release copper into the bloodstream. Zinc supplements can prevent the intestines from absorbing copper. Additionally, dietary changes to avoid foods high in copper are also recommended.
Apotemnophilia
Apotemnophilia, a rare paraphilic disorder, has intrigued psychologists and researchers for years. This condition involves individuals developing a strong sexual or erotic interest in the idea of being an amputee. In this article, we delve into the various aspects of apotemnophilia, its potential causes, and the ethical considerations surrounding it.
Apotemnophilia, also known as body integrity identity disorder (BIID), is characterized by an intense desire to amputate a healthy limb or have a limb amputated. Individuals with this condition often experience distress and a strong dissatisfaction with the presence of their limbs. They may fantasize about amputation, experience sexual arousal when imagining themselves as amputees, and may even attempt self-amputation.
The exact causes of apotemnophilia are not fully understood, but researchers have proposed various theories. Some suggest that it may be linked to a neurological condition affecting body image perception. Others believe it may be a form of body dysmorphic disorder or a manifestation of a deep-seated psychological issue. However, more research is needed to gain a comprehensive understanding of its origins.
Apotemnophilia raises ethical dilemmas regarding the treatment and support of individuals with this condition. While some argue that elective amputations should be allowed if they improve an individual’s quality of life, others believe that offering such procedures can perpetuate harmful behaviors. The medical community faces the challenge of balancing the autonomy of individuals with ethical considerations and ensuring the best possible care and support for those affected.
Apotemnophilia remains a complex and controversial condition that warrants further research and understanding. It is essential to approach this topic with empathy and compassion, recognizing the challenges faced by individuals with apotemnophilia. By fostering open discussions and supporting further studies, we can strive to provide the best care for those affected by this rare disorder.
Fregoli Delusion
Imagine living in a world where every face you see is just a mask, disguising the true identity of people around you. This is the perplexing reality for individuals suffering from Fregoli Delusion, a rare psychiatric disorder that distorts one’s perception of familiar faces. In this article, we will delve into the intricacies of Fregoli Delusion, exploring its symptoms, causes, and potential treatment options.
Fregoli Delusion, named after the Italian actor Leopoldo Fregoli, is a rare disorder characterized by the firm belief that different people are the same person in disguise. Those affected by this condition perceive others as impostors who are trying to deceive them. This delusion can extend beyond strangers, affecting relationships with family and friends as well.
Individuals experiencing Fregoli Delusion often exhibit various symptoms, including:
– Persistent and irrational belief that different people are the same person.
– Feeling constantly watched, stalked, or followed.
– Heightened sense of paranoia and suspicion.
– Anxiety and distress in social situations.
– Difficulty trusting others due to the fear of being deceived.
The exact cause of Fregoli’s Delusion remains unknown. However, it is believed to be associated with underlying neurological or psychiatric conditions, such as schizophrenia, brain injury, or dementia. Additionally, traumatic events, genetic predisposition, and abnormal brain functioning may contribute to the development of this rare disorder.
Diagnosing Fregoli Delusion can be challenging due to its rarity and similarity to other psychiatric disorders. Medical professionals rely on thorough psychiatric evaluations, interviews, and observation of symptoms to make an accurate diagnosis. Treatment typically involves a combination of medication, such as antipsychotics, and psychotherapy to address the underlying causes and manage symptoms effectively.
Fregoli Delusion is a fascinating and perplexing condition that challenges our understanding of perception and identity. The belief that familiar faces are mere illusions can have a profound impact on the lives of those affected. By increasing awareness and understanding of this disorder, we can provide support and empathy to individuals who experience the distressing effects of Fregoli Delusion. With further research and advancements in psychiatric care, we hope to unlock more effective treatment options and alleviate the burden faced by those living with this rare disorder.
Lesch-Nyhan Syndrome
Lesch-Nyhan Syndrome (LNS) is a rare genetic disorder that affects the development and function of the nervous system. Named after the physicians who first described it, Michael Lesch and William Nyhan, this syndrome primarily affects males. In this article, we will explore the causes, symptoms, and potential treatments for Lesch-Nyhan Syndrome.
LNS is caused by a mutation in the HPRT1 gene, which is responsible for producing an enzyme called hypoxanthine-guanine phosphoribosyltransferase (HGprt). This enzyme plays a crucial role in the recycling of purines, a necessary component of DNA and RNA. The HPRT1 gene mutation results in a deficiency or complete absence of HGprt enzyme activity, leading to the accumulation of uric acid and other substances in the body.
The symptoms of LNS usually become apparent during infancy or early childhood. The most characteristic feature of LNS is the presence of self-injurious behaviors, including biting fingers, lips, and other body parts. These behaviors are often triggered by involuntary muscle movements known as dystonia. Other symptoms may include intellectual disability, delayed motor development, gout, kidney stones, and abnormal muscle tone.
Currently, there is no cure for LNS, and treatment primarily focuses on managing symptoms and improving the quality of life for individuals with the syndrome. Medications such as allopurinol can help reduce uric acid levels and prevent complications like gout and kidney stones. Physical and occupational therapy can assist in improving motor skills, while behavioral therapy can help manage self-injurious behaviors.
Due to the rarity of LNS, support groups and organizations play a vital role in providing resources, information, and emotional support for affected individuals and their families. These groups also promote awareness and fund research initiatives aimed at understanding the syndrome better and developing possible treatments.
Lesch-Nyhan Syndrome is a rare genetic disorder that profoundly impacts the lives of those affected and their families. While there is no cure for LNS, advancements in research and medical interventions have improved the management of symptoms and quality of life for individuals with the syndrome. By raising awareness and supporting further research, we can continue to enhance our understanding of LNS and provide hope for affected individuals and their loved ones.
Turner Syndrome
Turner Syndrome is a genetic disorder that affects females. It occurs when one of the X chromosomes is partially or completely missing. This condition affects approximately 1 in every 2,500 female births. In this article, we will delve into the causes, symptoms, diagnosis, and treatment options for Turner Syndrome.
Turner Syndrome is caused by a random error during the formation of reproductive cells in either the mother or the father. The missing or altered X chromosome can result in a range of physical and developmental challenges.
The symptoms of Turner Syndrome can vary greatly from one individual to another. Common physical characteristics include short stature, a webbed neck, a low hairline at the back of the neck, and a broad chest with widely spaced nipples. Additionally, girls with Turner Syndrome may experience delayed puberty, infertility, heart abnormalities, and learning difficulties.
Diagnosing Turner Syndrome typically involves a physical examination, analysis of medical history and genetic testing. Prenatal screening and testing can also help identify the condition before birth. Early detection and intervention are crucial for managing the associated health issues effectively.
While there is no cure for Turner Syndrome, early intervention and comprehensive medical care can help manage the symptoms and improve quality of life. Treatment options may include growth hormone therapy to improve height, estrogen replacement therapy to induce puberty, and regular monitoring of heart and kidney function. Educational support and counseling play a vital role in addressing learning difficulties and psychological challenges.
Living with Turner Syndrome can present unique challenges, but with the right support and care, individuals can lead fulfilling lives. Regular medical check-ups, including cardiovascular assessments, are essential to prevent and manage associated health issues. Emotional and educational support, along with involvement in support groups, can help individuals and their families navigate the challenges that arise.
is a complex genetic disorder that affects females. While it presents unique challenges, early diagnosis, and comprehensive management can significantly improve the quality of life for individuals with Turner Syndrome. By raising awareness and providing support, we can create a more inclusive and understanding society for those affected by this condition.
Geographic Tongue
Geographic tongue, also known as benign migratory glossitis, is a harmless yet peculiar condition that affects the surface of the tongue. It is characterized by irregular, map-like patterns on the tongue’s surface, giving it a geographical appearance. While not a serious health concern, geographic tongue can cause discomfort and sensitivity. In this article, we will delve into the causes, symptoms, and potential treatment options for this intriguing condition.
The exact cause of geographic tongue remains unknown, making it difficult to prevent or predict. However, some studies suggest that there may be a genetic component involved. Other triggers include hormonal changes, stress, allergies, and certain dietary factors. It is important to note that geographic tongue is not contagious and cannot be transmitted through contact.
Geographic tongue often presents with various symptoms, including irregular-shaped patches on the tongue’s surface, varying in size and color. These patches may appear red, pink, or white, and can change in location and shape over time. Some individuals may experience a burning or stinging sensation, especially when consuming spicy or acidic foods. In rare cases, individuals may also experience mild discomfort or pain.
As the geographic tongue is a benign condition, treatment is typically focused on managing symptoms rather than curing the condition itself. Maintaining good oral hygiene practices, such as regular brushing and flossing, can help alleviate discomfort and reduce the risk of infection. Avoiding triggers, such as spicy or acidic foods, may also help minimize symptoms. In some cases, doctors may prescribe topical medications or mouth rinses to provide temporary relief.
Geographic tongue is a harmless yet intriguing condition that affects the surface of the tongue, resulting in irregular, map-like patterns. While the exact cause remains unknown, it is believed to have genetic and environmental triggers. Although there is no specific cure for the geographic tongue, managing symptoms through good oral hygiene practices and avoiding triggers can help ease discomfort. If you suspect you have a geographic tongue, it is always advisable to consult with a healthcare professional for an accurate diagnosis and appropriate treatment options.
In conclusion, the geographic tongue may be a peculiar condition, but with proper understanding and management, individuals can effectively navigate the discomfort associated with this unique condition.
Catatonic Schizophrenia
Catatonic schizophrenia is a rare and severe form of schizophrenia that affects a person’s ability to move and speak. It is characterized by a range of symptoms, including motor abnormalities, social withdrawal, and disorganized behavior. In this article, we will explore the symptoms, causes, and treatment options for catatonic schizophrenia.
Individuals with catatonic schizophrenia often exhibit a variety of symptoms that can be classified into two categories: positive and negative symptoms. Positive symptoms include hallucinations, delusions, and disorganized speech, whereas negative symptoms involve a loss of normal functions such as emotions, motivation, and social interaction. However, the hallmark of catatonic schizophrenia is the presence of catatonic features, which include stupor, mutism, posturing, and repetitive movements.
The exact cause of catatonic schizophrenia remains unknown, but it is believed to be a complex interplay of genetic, environmental, and neurochemical factors. Genetic predisposition plays a significant role, as individuals with a family history of schizophrenia are more likely to develop catatonic schizophrenia. Additionally, imbalances in brain chemicals, such as dopamine and serotonin, may contribute to the onset of this condition. Stressful life events and substance abuse can also trigger or worsen catatonic schizophrenia in susceptible individuals.
Treatment for catatonic schizophrenia usually involves a combination of medication, psychotherapy, and support. Antipsychotic medications are commonly prescribed to manage the positive symptoms, while mood stabilizers or antidepressants may be used to address associated mood disorders. Psychotherapy, such as cognitive-behavioral therapy, can help individuals develop coping strategies and improve their overall functioning. In severe cases, electroconvulsive therapy (ECT) may be considered to alleviate symptoms.
Catatonic schizophrenia is a debilitating condition that requires comprehensive treatment and ongoing support. Early detection and intervention are crucial for minimizing the impact of this disorder on individuals and their families. By raising awareness and understanding of catatonic schizophrenia, we can foster a greater sense of empathy and compassion for those affected by this complex mental illness. If you or someone you know is experiencing symptoms of catatonic schizophrenia seek professional help to receive an accurate diagnosis and appropriate treatment. Remember, with the right support, individuals with catatonic schizophrenia can lead fulfilling lives and achieve their full potential.
Body Dysmorphia
Body dysmorphia, also known as body dysmorphic disorder (BDD), is a mental health condition characterized by obsessive thoughts and preoccupations with one’s perceived flaws and imperfections. It affects individuals of all genders and ages and can have a significant impact on their quality of life. In this article, we will delve into the intricacies of body dysmorphia, its causes, symptoms, and available treatment options.
Body dysmorphia goes beyond mere dissatisfaction with one’s appearance. It involves distorted thinking patterns that lead individuals to exaggerate their flaws, often to the point of obsession. These perceived imperfections can range from minor blemishes to imagined deformities, causing significant distress and impairing daily functioning.
While the exact cause of body dysmorphia remains unknown, several factors contribute to its development. Genetics, brain chemistry, and environmental factors such as societal pressure and media influence play significant roles. Individuals with a history of trauma, abuse, or bullying may also be at a higher risk of developing body dysmorphia.
Recognizing the signs and symptoms of body dysmorphia is crucial for early intervention and support. Common indicators include excessive grooming or mirror-checking, seeking reassurance about one’s appearance, avoiding social situations, and engaging in repetitive behaviors such as skin picking or excessive exercise. Emotional distress, anxiety, and depression are often associated with the condition.
Treating body dysmorphia typically involves a combination of therapy and medication. Cognitive-behavioral therapy (CBT) is the most effective form of therapy, helping individuals challenge negative thought patterns and develop healthier coping strategies. Antidepressant medication may also be prescribed to manage associated symptoms of anxiety and depression.
If you suspect that someone you know is struggling with body dysmorphia, it is essential to approach the matter with empathy and understanding. Encourage open communication, offer support, and suggest seeking professional help. Remember, body dysmorphia is a serious condition that requires professional intervention.
Body dysmorphia is a complex mental health condition that affects millions of individuals worldwide. By understanding its causes, recognizing its signs, and promoting empathy and support, we can create a more inclusive and accepting society. Remember, true beauty lies not in the pursuit of perfection, but in embracing our uniqueness and individuality.
Hanahaki Disease
Hanahaki Disease is a fictional condition that has captured the imagination of many through its portrayal in literature and media.
The concept of Hanahaki Disease originated in Japanese folklore and has since gained popularity in modern storytelling. It is a fictional illness in which a person experiences severe coughing and vomiting of flower petals due to unrequited love. The flowers that manifest vary depending on the individual’s feelings and can range from roses, and lilies, to even more exotic blooms. As the disease progresses, the flowers grow in the lungs, leading to difficulty breathing and eventually death if the love remains unrequited.
Hanahaki Disease serves as a poignant metaphor for the pain and longing associated with unrequited love. The flowers that bloom within the afflicted person’s lungs represent the emotional burden they carry, unable to express their feelings or find closure. The physical manifestation of the disease mirrors the emotional turmoil experienced by those who pine for someone who cannot reciprocate their affection. It symbolizes the internal struggle between the heart and the mind, entwined in a battle of love and despair.
Although Hanahaki Disease is a fictional concept, its metaphorical significance has sparked discussions about the treatment of unrequited love. In many stories, the only cure for Hanahaki Disease is for the person’s love to be reciprocated or for the feelings to be extinguished completely. However, in reality, open communication, self-reflection, and seeking support from friends and loved ones can help individuals cope with unrequited love and find healing.
Hanahaki Disease may be a fictional condition, but its metaphorical significance resonates with many who have experienced unrequited love. Through its portrayal in literature and media, it serves as a reminder of the complexities of human emotions and the power of love. While the disease may not have a real-life cure, understanding its metaphorical implications can help individuals navigate the challenges of unrequited love with empathy and compassion.
Boanthropy
Have you ever heard of a rare psychological disorder called Boanthropy? Derived from the Greek words “boas” (meaning cow) and “anthropos” (meaning human), Boanthropy is a fascinating condition that involves a person’s delusion of transforming into a cow or another animal. This peculiar disorder has captivated the attention of psychologists, historians, and curious minds alike. In this article, we will delve into the intriguing world of Boanthropy, exploring its origins, symptoms, and potential explanations.
Boanthropy is not a recent development; it has been documented throughout history. Ancient Greek mythology tells tales of gods and goddesses turning people into animals as a form of punishment. In more recent times, cases of Boanthropy have been reported sporadically, with notable instances dating back to the 19th century.
Individuals suffering from Boanthropy experience a profound conviction that they have undergone a metamorphosis into a bovine creature or another animal. This delusion can manifest in various ways, such as adopting animalistic behaviors, believing they possess animal-like anatomy or even vocalizing sounds associated with the chosen animal. Patients may exhibit grazing behaviors, prefer grass as a dietary staple, and avoid social interaction with humans.
Psychologists and neurologists have proposed several theories to explain the underlying causes of Boanthropy. One hypothesis suggests that the disorder may be linked to a combination of psychological factors, including stress, trauma, and dissociative states. Additionally, some researchers speculate that Boanthropy could be a manifestation of a deeper identity crisis or a desire to escape from human responsibilities and pressures.
Treating Boanthropy can be challenging, as individuals with this disorder often lack insight into their delusions. Psychotherapy, specifically cognitive-behavioral therapy, has shown some success in helping patients challenge and modify their distorted beliefs. Medication, such as antipsychotics, may also be prescribed to address concurrent psychiatric conditions.
Boanthropy remains a perplexing psychological disorder that continues to intrigue both professionals and the general public. While relatively rare, its impact on those affected can be profound. Through further research and understanding, we hope to shed light on the complexities of Boanthropy and develop more effective interventions for those struggling with this condition. In the meantime, let us marvel at the mysteries of the human mind and its intricate manifestations.
Kluver-Bucy Syndrome
Kluver-Bucy Syndrome (KBS) is a rare neurological disorder that affects the brain’s ability to regulate emotions, behavior, and memory. It was first identified in the mid-20th century by the neurologists Heinrich Kluver and Paul Bucy. This syndrome is characterized by a set of distinctive symptoms, including hypersexuality, increased appetite, visual agnosia, and docility. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for Kluver-Bucy Syndrome.
KBS is primarily caused by damage to the temporal lobes of the brain, which are responsible for processing visual information and regulating emotions. This damage can occur due to various factors, such as viral infections, head trauma, tumors, or neurodegenerative diseases. Additionally, certain genetic factors may predispose individuals to develop KBS.
One of the hallmark symptoms of KBS is hypersexuality, where affected individuals may exhibit increased sexual activity, inappropriate sexual behavior, and a lack of sexual inhibition. Other symptoms include a significant increase in appetite, leading to overeating and weight gain. Visual agnosia, the inability to recognize objects or faces, is another common symptom. Additionally, individuals with KBS may display docility, where they become socially withdrawn and exhibit reduced aggression.
Diagnosing KBS can be challenging, as its symptoms can mimic those of other neurological disorders. A comprehensive medical history, physical examination, and neurological testing are crucial for an accurate diagnosis. Brain imaging techniques like Magnetic Resonance Imaging (MRI) or Computerized Tomography (CT) scans can help identify any structural abnormalities in the brain that may be associated with KBS.
There is no specific cure for KBS, and treatment primarily focuses on managing the symptoms and improving the individual’s quality of life. Medications, such as antidepressants, antianxiety drugs, and antipsychotics, may be prescribed to address behavioral and emotional issues. Cognitive-behavioral therapy and psychotherapy can also be beneficial in helping individuals cope with their symptoms and develop appropriate social skills.
Kluver-Bucy Syndrome is a rare neurological disorder that presents a unique set of symptoms related to behavioral, emotional, and cognitive functioning. While it can significantly impact an individual’s life, early diagnosis and appropriate management can help individuals with KBS lead fulfilling lives. Further research is necessary to gain a deeper understanding of the underlying causes and potential treatment options for this rare disorder. By raising awareness and promoting research, we can enhance the lives of those affected by Kluver-Bucy Syndrome and their families.
Imposter Syndrome
Imposter Syndrome is a psychological phenomenon that affects individuals from all walks of life. It is characterized by persistent feelings of self-doubt and a fear of being exposed as a fraud, despite evidence of one’s competence and accomplishments. In this article, we will explore the causes and effects of Imposter Syndrome and discuss practical strategies to overcome it.
Imposter Syndrome can manifest in various ways, including the fear of failure, perfectionism, and the belief that success is attributed solely to luck or external factors. Often, individuals experiencing this syndrome downplay their achievements, attributing them to chance rather than acknowledging their capabilities. This self-doubt can hinder personal and professional growth, leading to missed opportunities and a constant cycle of anxiety and dissatisfaction.
Several factors contribute to the development of Imposter Syndrome. High-achievers, perfectionists, and individuals transitioning into new roles or industries are particularly susceptible. Childhood experiences, societal pressures, and negative self-talk can also contribute to feelings of inadequacy. The effects of Imposter Syndrome include increased stress, decreased self-confidence, and a reluctance to take on new challenges or pursue higher goals.
Imposter Syndrome is a common struggle faced by many individuals, but it doesn’t have to define your life or hinder your success. By recognizing your achievements, challenging negative self-talk, seeking support, and embracing continuous learning, you can overcome Imposter Syndrome and unlock your full potential. Remember, you are capable, deserving, and unique in your own right. Embrace your true self and let go of self-doubt. Your accomplishments are a testament to your abilities, and the world is waiting to witness your greatness.
Histrionic Personality Disorder
Histrionic Personality Disorder (HPD) is a complex psychological condition characterized by attention-seeking behavior, exaggerated emotions, and a constant need for validation. In this article, we will delve into the causes, symptoms, and treatment options available for individuals with HPD.
The exact cause of Histrionic Personality Disorder is not fully understood. However, it is believed to be influenced by a combination of genetic, environmental, and social factors. Individuals with a family history of mental health disorders, such as HPD or borderline personality disorder, may have an increased risk. Additionally, traumatic life experiences, such as neglect or abuse during childhood, can contribute to the development of HPD. Cultural and societal influences may also play a role in shaping personality traits associated with this disorder.
People with HPD often display excessive emotionality, seeking constant attention and approval from others. They may exhibit dramatic behavior, often drawing attention to themselves through their appearance, speech, or actions. Individuals with HPD may have difficulty maintaining healthy relationships, as their intense emotions and need for validation can be overwhelming for others. They may also be prone to impulsive decisions and tend to exaggerate or fabricate stories to gain attention.
Treatment for Histrionic Personality Disorder typically involves a combination of psychotherapy, medication, and support from loved ones. Psychotherapy, such as cognitive-behavioral therapy (CBT) or dialectical behavior therapy (DBT), can help individuals with HPD gain insight into their thoughts and behaviors, develop healthier coping mechanisms, and improve their interpersonal skills. In some cases, medication may be prescribed to manage associated symptoms, such as depression or anxiety. Building a strong support network and fostering healthy relationships are also crucial aspects of managing HPD.
Histrionic Personality Disorder can significantly impact an individual’s life, but with proper diagnosis, understanding, and treatment, individuals with HPD can learn to manage their symptoms and lead fulfilling lives. If you suspect you or someone you know may have HPD, it is essential to seek the guidance of a mental health professional for an accurate assessment and appropriate treatment options.
Cyclothymic Disorder
Cyclothymic Disorder is a lesser-known mood disorder characterized by recurrent mood swings that fluctuate between periods of hypomania and mild depression.
Individuals with Cyclothymic Disorder experience mood swings that are less severe than those associated with bipolar disorder but still disruptive to their daily lives. During hypomanic episodes, they may feel euphoric, energetic, and excessively talkative. Conversely, during depressive episodes, they may experience feelings of sadness, hopelessness, and a lack of interest in activities. These mood swings typically last for at least two years in adults, with periods of stable mood lasting less than two months.
The exact cause of Cyclothymic Disorder is unknown, but it is believed to be influenced by a combination of genetic, biological, and environmental factors. Family history plays a significant role, as individuals with relatives who have bipolar disorder or Cyclothymic Disorder are at a higher risk. Imbalances in brain chemicals, such as serotonin and dopamine, may also contribute to the development of this disorder. Additionally, stressful life events or chronic stress can trigger or exacerbate symptoms.
Cyclothymia can be effectively managed with a combination of psychotherapy and medication. Psychotherapy, such as cognitive-behavioral therapy (CBT) or dialectical behavior therapy (DBT), can help individuals develop coping strategies, regulate their moods, and improve their overall well-being. Medications, such as mood stabilizers or antidepressants, may be prescribed to help manage mood swings. Individuals with Cyclothymic Disorder need to establish a consistent routine, prioritize self-care, and seek support from loved ones.
Cyclothymic Disorder is a chronic condition that requires ongoing management, but with the right treatment and support, individuals can lead fulfilling lives. If you suspect you or someone you know may have Cyclothymic Disorder, it is crucial to consult with a mental health professional for a proper diagnosis and to discuss appropriate treatment options.
Moebius Syndrome
Moebius Syndrome is a rare congenital neurological disorder characterized by facial paralysis and impaired lateral eye movement. Named after the German neurologist Paul Julius Moebius, who first described it in 1888, this condition affects about 1 in 50,000 to 1 in 500,000 newborns worldwide.
Individuals with Moebius Syndrome often display a mask-like facial expression due to underdeveloped or absent facial nerves. This paralysis results in an inability to smile, frown, or raise their eyebrows, significantly impacting non-verbal communication. Additionally, those affected struggle with eye movements, specifically lateral (side-to-side) motion, which can lead to strabismus (crossed eyes) and other vision issues.
The exact cause of Moebius Syndrome remains unclear, though it is believed to result from a combination of genetic and environmental factors affecting the development of cranial nerves during early pregnancy. Some cases have been linked to mutations in specific genes, while others may be associated with maternal factors such as diabetes or certain medications taken during pregnancy.
Diagnosis of Moebius Syndrome is primarily clinical, based on physical symptoms and medical history. Magnetic Resonance Imaging (MRI) and electromyography (EMG) can support the diagnosis by revealing abnormalities in the cranial nerves and muscles.
While there is no cure for Moebius Syndrome, various treatments can help manage symptoms and improve quality of life. Surgical interventions, such as muscle and nerve transplants, can restore some facial movement. Physical and occupational therapies enhance motor skills and daily functioning, while speech therapy aids in overcoming difficulties with speech and feeding.
Living with Moebius Syndrome presents unique challenges, but with proper support and medical care, individuals can lead fulfilling lives. Raising awareness about this condition is crucial to foster understanding and support for those affected, ensuring they receive the necessary resources and opportunities to thrive.
Hoarding Disorder
Hoarding Disorder is a complex mental health condition characterized by persistent difficulty in discarding or parting with possessions, regardless of their actual value. This behavior leads to the accumulation of items, often resulting in cluttered living spaces that can significantly impair daily functioning and pose health and safety risks.
The causes of Hoarding Disorder are multifaceted, involving a combination of genetic, environmental, and psychological factors. It often coexists with other mental health conditions such as anxiety, depression, and Obsessive-Compulsive Disorder (OCD). Traumatic events and significant life stressors can also trigger or exacerbate hoarding behaviors.
Individuals with Hoarding Disorder experience intense distress at the thought of discarding items. This distress is often rooted in a perceived need to save items for future use or sentimental reasons. Over time, the accumulation of items can overwhelm living spaces, making them difficult to navigate and increasing the risk of falls, fire hazards, and health issues.
Treatment for Hoarding Disorder typically involves a combination of cognitive-behavioral therapy (CBT) and, in some cases, medication. CBT helps individuals understand the underlying causes of their hoarding behaviors and develop healthier coping mechanisms. Support from family, friends, and support groups can also be invaluable in managing the disorder.
Raising awareness about Hoarding Disorder is essential to reducing stigma and encouraging those affected to seek help. With proper treatment and support, individuals with Hoarding Disorder can regain control over their lives and create safer, more manageable living environments.
Stiff Person Syndrome
Stiff Person Syndrome (SPS) is a rare and often debilitating neurological disorder characterized by severe muscle stiffness and spasms. This condition, which affects about one in a million people, can lead to significant mobility issues and chronic pain, severely impacting the quality of life.
SPS primarily affects the muscles of the trunk and limbs, causing them to become rigid and prone to painful spasms. These symptoms can be triggered by various factors, including sudden movements, stress, or even loud noises. The stiffness and spasms often lead to abnormal postures and an increased risk of falls and injuries.
The exact cause of Stiff Person Syndrome remains unclear, but it is believed to be an autoimmune disorder. In many cases, individuals with SPS have elevated levels of antibodies that attack a protein involved in nerve function, disrupting normal muscle control. This autoimmune response is often associated with other conditions, such as diabetes or thyroiditis.
Diagnosis of SPS is challenging due to its rarity and the similarity of its symptoms to other neurological disorders. It typically involves a combination of clinical evaluations, blood tests for specific antibodies and electromyography (EMG) to assess muscle activity.
Treatment for SPS focuses on managing symptoms and improving quality of life. This may include medications to relax muscles and reduce spasms, such as benzodiazepines and muscle relaxants, as well as physical therapy to maintain mobility and strength. In some cases, immunotherapy may be used to target the underlying autoimmune response.
Awareness and understanding of Stiff Person Syndrome are crucial for early diagnosis and effective management, offering hope and improved outcomes for those affected by this challenging condition.
Acrophobia
Acrophobia, the intense fear of heights, is a common phobia affecting millions of people worldwide. This fear can manifest as anxiety, dizziness, sweating, and even panic attacks when faced with high places or the mere thought of them.
The roots of acrophobia can be traced to both genetic and environmental factors. Evolutionarily, a fear of heights makes sense as a protective mechanism against falls and injury. However, personal experiences, such as a traumatic fall or witnessing someone else’s accident, can also trigger this phobia. Additionally, some studies suggest that individuals with anxiety disorders may be more prone to developing acrophobia.
Symptoms of acrophobia vary in severity. For some, standing on a ladder or looking out of a high window can induce mild unease, while others might experience debilitating fear even when safely on the ground but contemplating heights. This can significantly impact daily life, limiting activities and social interactions.
Treatment for acrophobia often involves cognitive-behavioral therapy (CBT), which helps individuals reframe their thoughts about heights and gradually expose themselves to high places in a controlled and safe manner. Virtual reality therapy is an emerging tool that provides realistic simulations to help patients confront their fears without physical risk.
Mindfulness and relaxation techniques, such as deep breathing and meditation, can also be effective in managing anxiety associated with heights.
Raising awareness about acrophobia is essential to fostering understanding and support for those affected. With proper treatment and coping strategies, individuals with acrophobia can overcome their fear and lead fuller, more adventurous lives.
Excoriation Disorder
Excoriation Disorder, also known as Dermatillomania or skin-picking disorder, is a mental health condition characterized by the compulsive urge to pick at one’s skin, leading to noticeable damage. This behavior, which affects about 1-2% of the population, often results in significant physical and psychological distress.
Individuals with Excoriation Disorder may pick at healthy skin, minor skin irregularities, or perceived imperfections, often spending several hours a day engaged in this behavior. The common areas affected include the face, arms, and hands. The repetitive nature of skin-picking can lead to infections, scarring, and severe tissue damage, as well as shame, guilt, and social withdrawal due to the visible effects on one’s appearance.
The exact cause of Excoriation Disorder is not fully understood, but it is believed to involve a combination of genetic, neurological, and environmental factors. It is often associated with other mental health conditions such as Obsessive-Compulsive Disorder (OCD), anxiety, and depression.
Treatment for Excoriation Disorder typically involves cognitive-behavioral therapy (CBT), which helps individuals identify and modify the thoughts and behaviors that contribute to skin-picking. Habit reversal training, a component of CBT, teaches alternative behaviors to replace skin-picking. In some cases, medications such as selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help manage underlying anxiety or depression.
Increasing awareness and understanding of Excoriation Disorder is crucial for reducing stigma and encouraging those affected to seek help. With appropriate treatment and support, individuals can manage their symptoms, improve their skin health, and enhance their overall well-being.
Triple X Syndrome
Triple X Syndrome, also known as Trisomy X or 47. Triple X Syndrome is a genetic condition that affects approximately 1 in 1,000 females. This syndrome occurs when a female has three X chromosomes instead of the usual two, resulting from a random error in cell division.
Many females with Triple X Syndrome may not exhibit noticeable symptoms and often lead typical lives. However, some may experience mild to moderate effects, including taller stature, learning disabilities, and delayed development of speech and motor skills. In some cases, there may be an increased risk of anxiety, attention deficit disorder (ADD), and other emotional or behavioral issues.
The diagnosis of Triple X Syndrome is usually made through a chromosomal analysis called karyotyping, often conducted when developmental delays or other related symptoms prompt medical investigation. Prenatal diagnosis is also possible through procedures like amniocentesis.
While there is no cure for Triple X Syndrome, early intervention and supportive therapies can help manage symptoms and enhance quality of life. Educational support, speech therapy, and physical therapy are commonly recommended to address developmental challenges. Psychological counseling may also be beneficial in managing emotional and behavioral issues.
Raising awareness about Triple X Syndrome is vital for promoting understanding and providing adequate support to those affected. With appropriate care and resources, individuals with Triple X Syndrome can thrive and lead fulfilling lives.
Savant Syndrome
Savant Syndrome is a rare mental disorder in which individuals with developmental disorders, such as autism, display profound and prodigious capabilities in specific areas like mathematics, music, art, or memory. This syndrome is estimated to occur in about 1 in 10 individuals with autism, but it can also manifest in people with other developmental or brain injuries.
People with Savant Syndrome often possess what are termed “islands of genius”—areas of exceptional talent that stand in stark contrast to their overall limitations. For example, a savant might be able to play a musical piece flawlessly after hearing it only once, solve complex mathematical problems in their head, or recall vast amounts of detailed information effortlessly. These extraordinary abilities are usually apparent from a young age and continue to develop with time.
The origins of Savant Syndrome are not fully understood. Some theories suggest that the brain compensates for damage or developmental anomalies by enhancing other cognitive functions. In particular, there is evidence that the right hemisphere of the brain, often associated with artistic and spatial abilities, may play a significant role.
While there is no specific treatment for Savant Syndrome, fostering the unique talents of individuals with this condition is crucial. Supportive environments that nurture their extraordinary abilities can lead to significant personal satisfaction and, in some cases, contributions to society.
Raising awareness about Savant Syndrome is essential for recognizing and appreciating the incredible potential within these individuals. Understanding and support can help them maximize their talents and lead enriched, fulfilling lives.


22 thoughts on “Unveiling 20 Rare Mental Disorders”