What Is Body Dysmorphia?

Body Dysmorphic Disorder (BDD) or Body Dysmorphia stands as a poignant reminder of the intricate interplay between perception, cognition, and mental health. Beyond the surface level of dissatisfaction with one’s appearance lies a profound and often debilitating condition characterized by obsessive thoughts and compulsive behaviors. This article embarks on a journey to deepen our understanding of BDD by delving into its definition, historical context, and prevalence to foster empathy and promote informed discourse on this complex disorder.
Definition of Body Dysmorphic Disorder
What Body Dysmorphia?
At its core, BDD involves an overwhelming preoccupation with perceived flaws in physical appearance, ranging from minor imperfections to entirely imagined defects. Individuals with BDD experience distressing thoughts and beliefs about their appearance, which often lead to compulsive behaviors aimed at concealing or correcting these perceived flaws. These behaviors, such as excessive grooming, mirror-checking, or seeking reassurance, serve as coping mechanisms but ultimately perpetuate the cycle of distress and dysfunction.
What distinguishes BDD from mere dissatisfaction with one’s appearance is the intensity and persistence of these concerns, coupled with significant impairment in social, occupational, and other areas of functioning. Despite reassurance from others or evidence to the contrary, individuals with BDD remain convinced of their perceived flaws, leading to profound emotional distress and diminished quality of life.
Body Dysmorphia History
The historical roots of BDD can be traced back to ancient civilizations, where references to individuals preoccupied with physical appearance can be found in philosophical texts and cultural narratives. However, in the late 19th century, BDD began to garner attention from the medical community. Enrico Morselli’s seminal work on dysmorphophobia laid the foundation for the conceptualization of BDD as a distinct psychiatric disorder characterized by obsessive concerns about bodily defects.
Over the following decades, clinicians and researchers defined the clinical features of BDD. They officially recognized it as a mental disorder in diagnostic manuals like the DSM. Despite its historical recognition, BDD remained relatively overlooked until the latter half of the 20th century, when advancements in psychiatric research and diagnostic criteria propelled it into the spotlight as a clinically significant disorder.
Frequency of Body Dysmorphic Disorder
Estimating the prevalence of BDD presents inherent challenges, given its secretive nature and overlap with other psychiatric conditions. Epidemiological studies suggest that BDD affects approximately 1-2% of the general population, with comparable rates across genders. However, due to underreporting, misdiagnosis, and societal stigma surrounding mental health, the true prevalence of BDD is likely underestimated by the figures.
Moreover, BDD often co-occurs with other psychiatric disorders, particularly mood and anxiety disorders, further complicating diagnosis and treatment. The onset of BDD typically occurs during adolescence or early adulthood, highlighting the critical need for early detection and intervention to mitigate long-term consequences and improve outcomes.
Body Dysmorphic Disorder represents a complex interplay of psychological, cognitive, and sociocultural factors, underscoring the importance of a multidimensional approach to understanding and addressing this condition. By elucidating BDD’s definition, historical evolution, and prevalence, we aim to destigmatize the disorder and foster greater empathy and support for individuals grappling with its profound impact.
It is crucial to prioritize research, education, and advocacy to raise awareness about BDD and promote early intervention and effective treatment strategies. By understanding BDD and working collaboratively, we can create a supportive environment to enhance the well-being of those impacted.
Body Dysmorphic Disorder Symptoms
Body Dysmorphic Disorder (BDD) is a multifaceted mental health condition that manifests through a spectrum of symptoms, each contributing to the profound distress and impairment experienced by affected individuals. This comprehensive exploration delves into the intricate tapestry of symptoms associated with BDD, shedding light on the complexity of this often-overlooked disorder.
1. Obsessive Preoccupation with Appearance
At the heart of BDD lies an overwhelming preoccupation with perceived flaws in physical appearance. This obsession consumes individuals’ thoughts, leaving them unable to focus on anything else. Whether it’s a perceived imperfection in their skin, facial features, or body shape, individuals with BDD find themselves endlessly fixating on these flaws, unable to escape the relentless cycle of negative thoughts and self-criticism.
2. Distorted Body Image
BDD distorts the way individuals perceive themselves, leading to a skewed body image that is detached from reality. Minor flaws are magnified and exaggerated, while positive aspects of one’s appearance are overlooked or dismissed. This distorted body image fuels feelings of inadequacy and self-loathing, perpetuating the cycle of obsession and anxiety.
3. Compulsive Behaviors
To cope with the distress caused by their perceived flaws, individuals with BDD often engage in compulsive behaviors aimed at either concealing or correcting these perceived imperfections. These behaviors may include excessive grooming, repetitive checking of one’s appearance in mirrors or reflective surfaces, seeking reassurance from others, or even undergoing unnecessary cosmetic procedures. While these behaviors may provide temporary relief, they ultimately reinforce the individual’s preoccupation with their appearance and exacerbate their distress.
4. Avoidance of Social Situations
The shame and embarrassment associated with their appearance concerns often lead individuals with BDD to avoid social situations or activities where their perceived flaws may be exposed. This avoidance can range from avoiding social gatherings and events to withdrawing from intimate relationships. The fear of judgment and scrutiny from others further isolates individuals with BDD, exacerbating their feelings of loneliness and alienation.
5. Impairment in Occupational and Social Functioning
The pervasive nature of BDD symptoms can significantly impair an individual’s ability to function in both occupational and social settings. The constant preoccupation with appearance may interfere with work performance, leading to absenteeism, decreased productivity, or even job loss. Similarly, strained relationships and social withdrawal can further isolate individuals with BDD, undermining their ability to maintain meaningful connections and engage in fulfilling activities.
6. Emotional Distress
Living with BDD takes a profound toll on one’s emotional well-being, leading to feelings of sadness, anxiety, and despair. The constant self-criticism and negative thoughts erode self-esteem and undermine one’s self-worth. Coping with the emotional turmoil of BDD can feel like an uphill battle, with each day presenting new challenges and obstacles to overcome.
7. Relationship Strain
BDD can strain relationships, as the preoccupation with appearance often takes precedence over other aspects of life. Loved ones may struggle to understand or empathize with the magnitude of distress experienced by individuals with BDD, leading to frustration and conflict. Communication breakdowns and feelings of alienation may further strain interpersonal relationships, exacerbating the sense of isolation and loneliness experienced by individuals with BDD.
8. Suicidal Thoughts and Behaviors
In severe cases, BDD can lead to suicidal thoughts and behaviors. The overwhelming distress and hopelessness experienced by individuals with BDD may leave them feeling as though there is no escape from their perceived flaws. Suicidal ideation may serve as a desperate attempt to end their suffering and find relief from the relentless torment of BDD. It is crucial to recognize the severity of these symptoms and intervene promptly to prevent tragic outcomes.
Variations and Severity in Symptoms
- Fluctuating Intensity: Symptoms of BDD may not be constantly severe. Stress, social events, or other triggers can worsen preoccupations and compulsive behaviors.
- Shifting Focus: Over time, the specific parts of the body an individual fixates on might change.
- Muscle Dysmorphia: A subtype of BDD where the obsession centers on perceived lack of muscle mass or definition, leading to compulsive bodybuilding and potential eating disorder behaviors.
Distinguishing BDD from Related Conditions
- Ordinary Self-Consciousness: Everyone occasionally experiences some degree of dissatisfaction with their appearance. BDD is about intensity, persistence, and the level of disruption it causes.
- Eating Disorders: While body image is often a component of eating disorders, BDD is characterized by a particular focus on individual features rather than overall weight and shape.
- Social Anxiety: Social phobia can involve appearance concerns, but BDD has a more extreme, all-consuming nature with compulsive behaviors that go beyond general worry about social interactions.
Body Dysmorphic Disorder encompasses a wide range of symptoms that permeate every aspect of an individual’s life. By understanding the diverse manifestations of BDD symptoms, we can better appreciate the profound impact of this disorder and provide support and intervention to those in need. Early detection, compassionate care, and evidence-based treatment approaches are essential in alleviating the burden of BDD and fostering recovery and resilience.
Body Dysmorphia Types
What are Body Dysmorphia types?
1. Skin Dysmorphia
Individuals with skin-related body dysmorphia often experience distress related to perceived flaws such as acne, scars, wrinkles, or blemishes. They may engage in excessive mirror checking, skin picking (dermatillomania), or spending excessive time and money on skincare products and treatments. Perceived imperfections can significantly impact self-esteem and quality of life, leading to avoiding social situations and impairing daily functioning.
2. Hair Dysmorphia
Hair-related body dysmorphia involves an obsessive preoccupation with the appearance of one’s hair. This can include concerns about hair thickness, texture, or perceived bald spots. Individuals may spend excessive time styling their hair, frequently change hairstyles or hair color, or invest in expensive hair treatments or hairpieces. Experiencing hair loss can be distressing and cause self-consciousness.
3. Facial Features Dysmorphia
This type of body dysmorphia focuses on perceived flaws in facial features such as the nose, eyes, lips, or jawline. Individuals may obsessively scrutinize their faces in mirrors, seek reassurance from others, or undergo repeated cosmetic procedures to correct perceived imperfections. Social interactions may be affected as individuals feel self-conscious about their appearance and avoid situations where their face is the center of attention.
4. Body Size and Shape Dysmorphia
Body dysmorphia related to body size and shape involves an intense preoccupation with weight, body fat, muscle tone, or overall body proportions. Individuals may have a distorted perception of their bodies, seeing themselves as more significant or more out of shape than they are. This can lead to extreme behaviors related to dieting, exercise, and avoidance of activities that involve exposing their bodies, such as swimming and intimate relationships.
5. Muscle Dysmorphia (Bigorexia)
Muscle dysmorphia, also known as “bigorexia,” is characterized by an obsession with muscularity and body size. Individuals with this subtype may perceive themselves as small or underdeveloped despite evidence to the contrary. They may engage in excessive weightlifting, follow strict diets, or misuse anabolic steroids or other performance-enhancing substances in pursuit of their desired physique. This obsession with muscularity can have negative impacts on physical and mental well-being, as well as relationships with others.
6. Genital Dysmorphia
Individuals with genital dysmorphia obsess over the appearance or size of their genitals. They may believe that their genitals are too small, asymmetrical, or otherwise abnormal, leading to feelings of shame, embarrassment, and inadequacy. This can significantly impact self-esteem and sexual relationships, leading to avoidance of intimacy and social withdrawal.
7. Height Dysmorphia
Height dysphoria involves an excessive concern about one’s height, with individuals perceiving themselves as too tall or too short. Height-related body dysmorphia can lead to feelings of insecurity, social anxiety, and avoidance of situations where height may be a focal point of attention, such as public speaking or dating. Height dysphoria can also impact self-image and interpersonal relationships, contributing to feelings of inadequacy and low self-worth.
8. Breast or Chest Dysmorphia
This subtype of body dysmorphia is characterized by an obsessive preoccupation with the size, shape, or symmetry of one’s breasts or chest area. Both men and women may experience distress related to their chest appearance, which can impact self-esteem, body image, and social functioning. Individuals may avoid certain clothing styles, intimate relationships, or social situations where their chest may be visible or scrutinized.
Overall, body dysmorphia can manifest in various forms and can significantly impact an individual’s emotional well-being, social interactions, and overall quality of life. It’s essential for individuals experiencing symptoms of body dysmorphia to seek professional help from a qualified mental health professional for accurate diagnosis and effective treatment. Managing body dysmorphic disorder and improving self-esteem can be achieved through therapy, medication, and support groups.
Body Dysmorphic Disorder Causes
Body Dysmorphic Disorder (BDD) stands as a testament to the intricate interplay of genetic, neurobiological, psychological, and environmental factors that contribute to the development of this debilitating condition. Understanding the underlying causes of BDD is crucial for elucidating its pathogenesis and informing targeted interventions. In this comprehensive analysis, we delve into the multifaceted etiology of BDD, shedding light on the diverse array of factors that may predispose individuals to this disorder.
1. Genetic Predisposition
Research suggests that BDD may be inherited, indicating an essential role of genetic factors in its susceptibility. Familial aggregation studies have revealed a higher prevalence of BDD among first-degree relatives of individuals with the disorder, suggesting a potential genetic predisposition. Genes linked to BDD, including those regulating neurotransmitters, serotonin, and neuroplasticity, have been identified through genome-wide association studies. However, the precise genetic mechanisms underlying BDD remain elusive and warrant further investigation.
2. Neurobiological Alterations
Neuroimaging studies have revealed significant insights into the neurobiological basis of BDD by highlighting changes in brain structure and function among affected individuals. Dysfunction in neural circuits implicated in body image processing, emotion regulation, and cognitive control has been observed in individuals with BDD. Specifically, abnormalities in regions such as the prefrontal cortex, insula, and striatum have been implicated in the distorted body image and obsessive thoughts characteristic of BDD. Dysregulation of neurotransmitter systems, including serotonin, dopamine, and glutamate, may further contribute to the pathophysiology of BDD.
3. Psychological Factors
Psychological factors like low self-esteem, perfectionism, and negative body image are critical in the development and maintenance of BDD. Individuals with BDD often harbor deep-seated insecurities about their appearance, stemming from early childhood experiences, societal pressures, or traumatic events. Maladaptive cognitive schemas, such as dichotomous thinking and selective attention to perceived flaws, contribute to the persistence of BDD symptoms. Additionally, comorbid psychiatric disorders, such as depression, anxiety, and obsessive-compulsive disorder, may exacerbate symptoms of BDD and complicate treatment.
4. Environmental Influences
Environmental factors, including societal influences, cultural norms, and interpersonal relationships, shape one’s perception of beauty and influence the development of BDD. In today’s image-centric society, where beauty ideals are often unrealistic and unattainable, individuals may feel immense pressure to conform to narrow standards of attractiveness. Exposure to social media, advertising, and peer comparisons can exacerbate feelings of inadequacy and fuel the desire for perfection, predisposing vulnerable individuals to the onset of BDD. Childhood experiences, such as childhood trauma, bullying, or parental criticism, may also contribute to the development of BDD later in life.
5. Co-occurring Mental Health Disorders
BDD commonly co-occurs with other psychiatric disorders, such as obsessive-compulsive disorder, depression, social anxiety disorder, and eating disorders. Shared underlying neurobiological and psychological mechanisms may underlie the co-occurrence of these disorders, contributing to the complexity of BDD presentation and treatment. Comorbid psychiatric conditions may exacerbate symptoms of BDD and necessitate a comprehensive, multidisciplinary approach to treatment.
- Not One Size Fits All The mix of contributing factors likely differs for each individual with BDD. There is no single “cause” that explains all cases.
- Blameless Condition: It’s vital to remember that individuals with BDD are not choosing their negative thoughts or engaging in compulsive behaviors out of vanity. There are underlying factors driving this distressing condition.
- Research Continues: As our understanding of the brain, genetics, and complex psychological influences deepens, so will our insights into the causes of BDD, potentially paving the way for more targeted prevention and treatment.
Body Dysmorphic Disorder is a multifaceted condition with a complex etiology involving a convergence of genetic, neurobiological, psychological, and environmental factors. By elucidating the diverse array of factors contributing to BDD, we can better understand its pathogenesis and inform targeted interventions to address the unique needs of affected individuals. Advancement of our understanding of BDD and the development of more effective treatments is promising, with future research endeavors focusing on unraveling the underlying mechanisms of this disorder.
Impacts of Body Dysmorphic Disorder
Body Dysmorphic Disorder (BDD) is not merely a superficial concern about one’s appearance; rather, it permeates every facet of an individual’s life, leaving a trail of profound and enduring consequences in its wake. From relentless psychological distress to the disruption of social relationships and occupational functioning, the impact of BDD reverberates far beyond the surface level. In this comprehensive exploration, we delve into the multifaceted repercussions of BDD, shedding light on the intricate web of challenges faced by individuals grappling with this debilitating disorder.
1. Emotional Distress and Psychological Turmoil
At the core of BDD lies a profound sense of emotional distress and psychological turmoil. Individuals afflicted with BDD are consumed by negative thoughts and feelings about their appearance, trapped in a perpetual cycle of self-criticism and inadequacy. The relentless scrutiny of perceived flaws breeds shame, embarrassment, and self-loathing, eroding self-esteem and undermining one’s self-worth. Coping with the emotional onslaught of BDD can feel like navigating a labyrinth of despair, with each twist and turn exacerbating the psychological burden borne by affected individuals.
2. Impaired Self-Perception and Self-Esteem
BDD distorts one’s self-perception, skewing how individuals view themselves and the world around them. Deep-seated insecurities about appearance lead to a distorted self-image characterized by a relentless focus on perceived flaws and imperfections. As a result, individuals with BDD may develop a skewed sense of self-esteem, oscillating between periods of unwarranted self-doubt and fleeting moments of fleeting confidence. The pervasive nature of BDD undermines self-assurance and self-worth, leaving individuals trapped in a cycle of self-deprecation and self-doubt.
3. Social Isolation and Interpersonal Strain
The impact of BDD extends beyond the individual to strain social relationships and foster feelings of isolation and alienation. The fear of being judged on appearance can lead to social isolation. Close relationships may suffer as loved ones struggle to understand or empathize with the magnitude of distress experienced by individuals with BDD. Communication breakdowns and strained relationships exacerbate feelings of loneliness and isolation, further perpetuating the cycle of social withdrawal and interpersonal strain.
4. Occupational and Academic Impairment
BDD can impair one’s ability to function effectively in academic and occupational settings, undermining productivity, performance, and career advancement. The preoccupation with appearance may distract individuals from their academic or professional responsibilities, leading to decreased concentration, absenteeism, and underachievement. Moreover, the psychological distress and emotional turmoil associated with BDD may interfere with job performance, jeopardizing career prospects and professional success. The impairment in occupational functioning exacerbates frustration, inadequacy, and self-doubt, hindering individuals’ ability to reach their full potential in academic and professional pursuits.
5. Financial Strain and Economic Burden
The financial burden of BDD extends beyond the individual to impose economic strain and hardship on families and caregivers. The financial burden of seeking treatment for BDD, including therapy, medication, and cosmetic procedures, can be substantial for individuals and their families. Moreover, the impairment in occupational functioning and reduced earning potential associated with BDD may exacerbate financial strain, leading to increased financial insecurity and economic hardship. The economic impact of BDD underscores the need for accessible and affordable treatment options to alleviate the financial burden affected individuals and their families bear.
6. Suicidal Ideation and Self-Harm Risk
In severe cases, BDD can precipitate suicidal ideation and self-harming behaviors, posing a grave risk to individuals’ safety and well-being. The overwhelming distress and hopelessness experienced by individuals with BDD may lead them to contemplate or attempt suicide as a means of escape from their perceived flaws and suffering. The shame and stigma associated with BDD may deter individuals from seeking help or disclosing their struggles, exacerbating feelings of isolation and despair. It is imperative to recognize the severity of these risks and intervene promptly to prevent tragic outcomes, providing comprehensive support and treatment to individuals grappling with BDD.
Body Dysmorphic Disorder leaves a lasting imprint on individuals’ lives, manifesting through a myriad of emotional, social, occupational, financial, and existential challenges. By unraveling the multifaceted repercussions of BDD, we can better appreciate its impact and develop targeted interventions to address the complex needs of affected individuals. It is essential to foster awareness, empathy, and support for those grappling with BDD, paving the way for recovery, resilience, and hope for a brighter future.
Body Dysmorphic Disorder Diagnosis
BDD can be a master of disguise, easily mistaken for typical self-consciousness or simply a fixation on looks. However, a thorough diagnostic process sheds light on the true extent of this complex disorder. Let’s delve deeper into professionals’ steps to identify BDD and accurately pave the way for appropriate support.
BDD Expertise: While many therapists are familiar with BDD, seeking a clinician specializing in OCD or body image issues offers the best chance of accurate diagnosis and understanding of the condition’s unique challenges.
Sensitivity and Patience: Discussing anxieties about one’s appearance can be profoundly uncomfortable. Finding a therapist who creates a safe, non-judgmental space is crucial for open communication.
Beyond the Surface: A skilled diagnostician looks beyond just the expressed symptoms. They probe to understand the emotional impact, the level of control the individual has over their thoughts, and how those thoughts influence daily life.
Diagnostic Tools
The Clinical Interview: Nuances Matter Beyond the core questions, a skilled clinician will explore:
-
- Fluctuations: Are there times when appearance concerns lessen? Do specific situations or stressors exacerbate the preoccupation?
- Attempts to Resist: How hard does the individual try to fight obsessive thoughts or compulsions? Do they offer temporary relief or only intensify distress?
- Impact on Relationships: Have romantic relationships been strained? Is there withdrawal from social circles due to appearance-related fear?
- Cosmetic Procedures: Have any been pursued or considered due to BDD-driven beliefs about “fixing” imperfections?
Specialized Questionnaires: While scores on BDD questionnaires offer valuable insight, the accompanying explanations and examples the individual provides are equally important:
-
- Highlighting Specific Distortions: Responses illuminate the exact features the person focuses on and how they misinterpret their appearance.
- Uncovering Hidden Behaviors: Questions about rituals or avoidance might reveal private behaviors a person feels ashamed to admit initially.
The Complexity of Co-Occurring Conditions
Since BDD frequently co-exists with other mental health struggles, careful screening is vital:
- Identifying the Cycle: Often, the conditions exacerbate each other. For instance, BDD-related social anxiety might worsen depression, which further fuels negative thoughts about appearance.
- Treatment Implications: Knowing if depression, anxiety disorders, or OCD are present is crucial, as treatment may need to target all conditions simultaneously for the best outcome.
- Masking BDD: Sometimes, other conditions are more obvious initially. For example, someone presenting with severe social anxiety might minimize how much a distorted body image drives anxiety.
Facing Potential Challenges
- Shame and Minimization: Deeply ingrained shame can make it hard to open up fully about the extent of BDD symptoms. A therapist must gently probe while being supportive to get an accurate picture.
- Acceptance of Diagnosis: For individuals firmly convinced of their defects, accepting a BDD diagnosis can take time. Patience and focusing on the disruption caused by the condition (regardless of its label) can be a helpful initial step.
- Finding the Right Specialist: Unfortunately, not all mental health providers have extensive training in diagnosing BDD. Online resources or referrals from professional organizations focused on OCD or eating disorders can help locate specialists.
Additional Considerations
- Differentiation for Adolescents: Since self-consciousness is common during teen years, it’s vital to assess whether appearance concerns are developmentally appropriate or match the intensity, persistence, and interference indicative of BDD.
- Cultural Context Matters: Cultural beauty ideals can influence the specific areas of focus, but it’s important to distinguish genuine BDD from dissatisfaction stemming from societal pressures many people experience.
While confronting the reality of BDD can be emotionally challenging, a diagnosis offers a crucial turning point. It validates the struggle, reduces self-blame, and provides a roadmap for a targeted treatment approach. With the proper support, individuals with BDD can learn to challenge distorted thoughts, manage compulsive behaviors, and build a life where appearance concerns no longer hold them captive.
Body Dysmorphia Treatment
Body Dysmorphic Disorder (BDD) is a complex mental health condition that affects individuals’ perceptions of appearance, leading to increased distress and impairment in daily functioning. Fortunately, various evidence-based treatment strategies are available to help individuals manage and overcome BDD. These strategies empower them to lead fulfilling lives free from the constraints of negative body image. We will explore each treatment approach in greater detail, providing insights into their effectiveness and how they can be integrated into a holistic treatment plan for BDD.
1. Cognitive-Behavioral Therapy (CBT)
Cognitive-Behavioral Therapy (CBT) is a highly useful option for Body Dysmorphic Disorder (BDD) and is widely considered the most preferred approach by mental health professionals. This structured, goal-oriented therapy focuses on identifying and challenging distorted thoughts and beliefs about one’s appearance. Individuals learn to replace negative and irrational thoughts with more realistic and balanced perspectives through cognitive restructuring techniques. Additionally, behavioral interventions, such as exposure and response prevention, help individuals confront their fears and reduce avoidance behaviors related to body image concerns. CBT equips individuals with practical coping strategies to manage anxiety and distress associated with BDD, empowering them to regain control over their lives.
2. Medication
While therapy is the primary treatment modality for BDD, medication can be a valuable adjunctive approach for managing symptoms, particularly those related to anxiety and depression. Selective Serotonin Reuptake Inhibitors (SSRIs) relieve the symptoms of Body Dysmorphic Disorder (BDD). These medications function by raising serotonin levels in the brain, aiding mood regulation and decreasing obsessive thoughts about one’s physical appearance. Psychiatrists may recommend a blend of SSRIs and therapy to provide thorough treatment for people suffering from BDD.
3. Mindfulness-Based Interventions
Mindfulness-based interventions offer individuals with BDD valuable tools for managing distressing thoughts and emotions related to appearance. Mindfulness techniques, such as mindfulness meditation and deep breathing exercises, help individuals develop awareness of their thoughts and feelings without judgment. By practising mindfulness, individuals learn to observe their negative body image thoughts without becoming entangled, fostering acceptance and self-compassion. Mindfulness-based interventions promote emotional regulation and resilience, empowering individuals to navigate challenges easily.
4. Support Groups
Support groups play a vital role in the lives of individuals who have Body Dysmorphic Disorder (BDD). These groups help individuals feel less alone by connecting them with others who are going through the same struggles. Support group members can share practical advice and control strategies in a safe and supportive environment to express their concerns and feelings. This allows individuals to feel encouraged and supported by those who genuinely understand what they are going through. Additionally, support groups can serve as a platform for advocacy and awareness-raising, fostering understanding and acceptance of BDD within society.
5. Family Therapy
BDD can significantly impact relationships with family members, leading to misunderstandings, conflicts, and strained communication. Family therapy provides a supportive environment for educating loved ones about BDD and its effects. Therapists work with families to improve communication, foster empathy and understanding, and support individuals with BDD. By addressing family dynamics and promoting open dialogue, family therapy helps strengthen relationships and create a supportive environment for recovery.
6. Acceptance and Commitment Therapy (ACT)
ACT is a mindfulness-based approach that emphasizes accepting complex thoughts and emotions while committing to actions aligned with values and goals. In ACT, individuals learn to detach from their negative body image thoughts and pursue meaningful activities and relationships. ACT empowers individuals to pursue a fulfilling life beyond the constraints of BDD by cultivating psychological flexibility and resilience.
7. Body-Focused Exposure and Ritual Prevention (B-FERPT)
Body-Focused Exposure and Ritual Prevention (B-FERPT) is a specialized form of exposure therapy designed to address specific body image concerns in BDD. Through structured exposure exercises, individuals gradually confront feared body parts or situations, reducing avoidance behaviors and anxiety. Therapists provide guidance and support as individuals engage their fears in a controlled setting, helping them develop healthier coping mechanisms and build resilience in the face of distressing thoughts and feelings.
Effective treatment of Body Dysmorphic Disorder BDD requires a comprehensive and integrated approach that addresses the underlying cognitive, emotional, and behavioral processes driving the condition. By combining cognitive-behavioral therapy (CBT), medication, mindfulness-based interventions, support groups, family therapy, acceptance and commitment therapy (ACT), and body-focused exposure and ritual prevention (B-FERPT), individuals with BDD can experience significant improvements in their symptoms and overall well-being. Individuals with Body Dysmorphic Disorder (BDD) must seek help from qualified mental health professionals to receive an accurate diagnosis and tailored treatment plan. With dedication and support, those with BDD can begin the journey of healing and self-discovery, freeing themselves from the grip of this disorder and reclaiming their lives.
Famous People with Body Dysmorphic Disorder
1. Michael Jackson
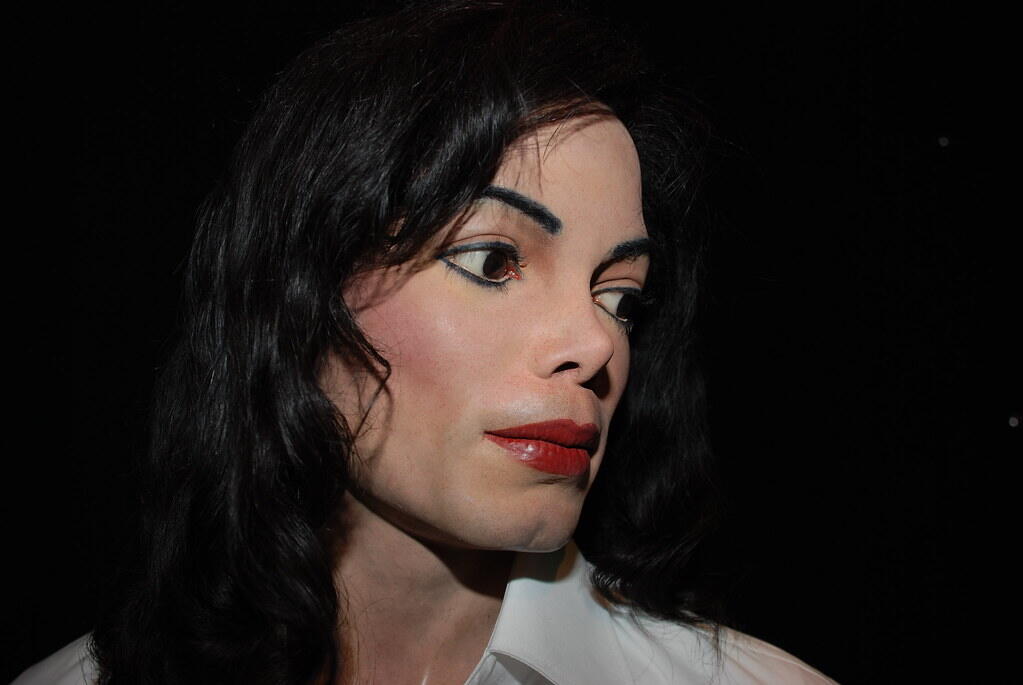
Michael Jackson, the legendary King of Pop, grappled with body dysmorphic disorder (BDD) throughout his life, leading to numerous cosmetic surgeries and alterations to his appearance.
Despite his unparalleled talent and global adoration, Jackson’s insecurities about his physical appearance were well-documented.
He underwent multiple surgeries on his nose, chin, and other facial features in an attempt to achieve what he perceived as perfection, leading to drastic changes in his appearance over the years.
Jackson’s struggle with BDD highlights the intense pressure faced by celebrities to meet society’s unrealistic beauty standards and the detrimental effects of body dysmorphia on mental health.
2. Joan Rivers
Joan Rivers, the groundbreaking comedian and television personality, openly discussed her lifelong battle with body dysmorphia.
Rivers was known for her self-deprecating humor regarding her numerous plastic surgeries, which she underwent in pursuit of a more youthful appearance.
Despite her success and acclaim in the entertainment industry, Rivers’ struggles with body image were a constant theme in her life, demonstrating the pervasive nature of BDD across different professions.
3. Nicole Kidman
Academy Award-winning actress Nicole Kidman has spoken candidly about her struggles with body dysmorphia, particularly during her early years in Hollywood.
Kidman has admitted feeling insecure about her appearance and has spoken about the pressure to maintain a specific image in the film industry.
Despite her talent and beauty, Kidman’s experiences highlight the problems faced by actors and actresses in an industry that often emphasizes physical appearance.
4. Harrison Ford
Harrison Ford, known for Star Wars and Indiana Jones, revealed battles with body dysmorphia.
Ford has spoken about feeling self-conscious about his looks, especially during his early years as an actor when he struggled to conform to Hollywood’s beauty standards.
Despite his status as a Hollywood legend, Ford’s experiences with BDD underscore the importance of self-acceptance and the detrimental effects of societal pressure on mental health.
5. Cindy Crawford
Supermodel Cindy Crawford, renowned for her beauty and success in the fashion industry, has been open about her struggles with body dysmorphia.
Crawford has spoken about feeling insecure about her appearance, particularly in an industry where physical perfection is highly valued.
Despite her success, Crawford’s experiences serve as a reminder of the pressures faced by models to maintain an unrealistic standard of beauty.
6. Eminem
Grammy-winning rapper Eminem has addressed his battles with body dysmorphia in his music and interviews.
Eminem has rapped about his insecurities and struggles with body image, providing a raw and honest portrayal of his personal experiences.
Despite his success in the music industry, Eminem’s openness about his struggles highlights the importance of destigmatizing mental health issues, particularly within the hip-hop community.
7. Sharon Osbourne
Television personality and businesswoman Sharon Osbourne has spoken candidly about her struggles with body dysmorphia.
Osbourne has undergone numerous plastic surgery procedures in an attempt to alter her appearance, reflecting the intense pressure faced by individuals in the public eye to meet society’s beauty standards.
Despite being successful, Osbourne’s experiences highlight the importance of mental health issues, regardless of fame or status.
8. Rob Lowe
Actor Rob Lowe has opened up about his battles with body dysmorphia.
Lowe has spoken about feeling self-conscious about his appearance, particularly during his early years as a heartthrob actor.
Despite his success, Lowe’s experiences underscore the importance of self-acceptance and the detrimental effects of societal pressure on mental health.
9. Victoria Beckham
Fashion designer and former Spice Girl Victoria Beckham has spoken about her struggles with body dysmorphia, particularly during her time in the music industry.
Beckham has admitted feeling insecure about her appearance and has spoken about the pressure to maintain a specific image in the public eye.
Despite being a fashion icon, Beckham’s experiences highlight the pervasive nature of Body Dysmorphic Disorder (BDD) and other mental health issues.
10. Elton John
Music legend Elton John has openly discussed his battles with body dysmorphia, particularly during his early years as a musician.
John has shared that he feels insecure about his appearance and the pressure to conform to societal beauty standards. Despite being a music icon, his experiences highlight the significance of self-acceptance and seeking support for mental health issues, regardless of one’s fame or success.


